Obstructive sleep apnea (OSA) is a common yet underdiagnosed sleep disorder affecting millions of people worldwide. Characterized by repeated interruptions in breathing during sleep, OSA can severely impact one’s health and quality of life. This article aims to provide a detailed understanding of the condition, its diagnosis, treatment options, and how it affects day-to-day living.
Overview of Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea (OSA) primarily affects adults, but it can also occur in children, particularly those with enlarged tonsils or obesity. The disorder is often categorized by the severity of symptoms, which can range from mild to severe.
|
Mild OSA |
5-14 apneic events per hour |
|
Moderate OSA |
15-30 events per hour |
|
Severe OSA |
Over 30 events per hour |
What is Obstructive Sleep Apnea (OSA)?
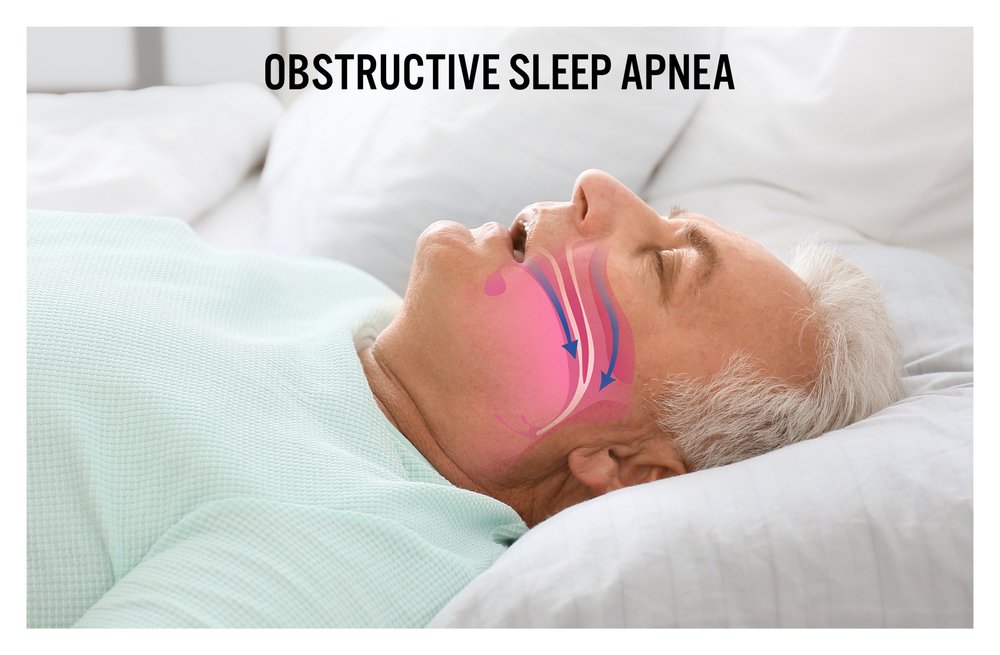
Obstructive sleep apnea (OSA) happens when the throat muscles relax too much during sleep, causing a temporary blockage of the airway. This blockage can lead to shallow breathing or pauses in breathing that last from a few seconds to a minute. Individuals with OSA may experience these interruptions multiple times per hour, leading to fragmented sleep and reduced oxygen levels.
OSA is more than just snoring or feeling exhausted during the day. It can cause significant health risks if left untreated, including cardiovascular disease, hypertension, stroke, and type 2 diabetes. According to the American Academy of Sleep Medicine, about 26% of adults aged 30-70 are estimated to suffer from OSA, making it one of the most prevalent sleep disorders.
Types of Sleep Apnea
Obstructive sleep apnea (OSA) is the most common form of sleep apnea, but there are other types to be aware of
- Obstructive sleep apnea (OSA): Obstructive sleep apnea (OSA) is the result of a physical obstruction.
- Central sleep apnea (CSA): The brain fails to send proper signals to the muscles that control breathing, resulting in breathing interruptions.
- Complex sleep apnea syndrome: Complex sleep apnea syndrome, also called treatment-emergent central sleep apnea, occurs when a person experiences both OSA and CSA simultaneously.
Causes of Obstructive Sleep Apnea (OSA)
Several factors contribute to the development of OSA, and it is usually a combination of anatomical and lifestyle factors. Common causes include:
- Excess weight: Individuals with obesity have a higher risk due to fat deposits around the upper airway, which can obstruct breathing.
- Narrowed Airway: Some people inherit naturally narrower airways or have enlarged tonsils or adenoids that block airflow.
- Neck circumference: A thicker neck can increase the likelihood of airway obstruction.
- Aging: The natural aging process causes a loss of muscle tone, including in the throat, increasing the risk of OSA.
- Family history: Genetics plays a role, as OSA can run in families.
- Alcohol or sedatives: These substances relax the muscles in the throat, exacerbating airway blockages.
Symptoms of OSA
The symptoms of obstructive sleep apnea (OSA) can vary, but the most common signs include
- Loud snoring (often noticed by bed partners)
- Pauses in breathing during sleep (sometimes accompanied by gasping or choking)
- Excessive daytime sleepiness (hypersomnia)
- Morning headaches
- Difficulty concentrating
- Irritability or mood changes
- Dry mouth or sore throat upon waking
These symptoms are often exacerbated by alcohol consumption, sedative use, or sleeping on one’s back, which can further relax the throat muscles and worsen airway obstruction.
Diagnosis of OSA
Diagnosing obstructive sleep apnea (OSA) involves a comprehensive evaluation by a healthcare professional, typically a sleep specialist. The most common diagnostic tool is polysomnography, or sleep study, which monitors brain activity, blood oxygen levels, heart rate, and breathing patterns while you sleep. Home sleep apnea tests are also available for those who may not require an in-lab study.
Based on the results, the severity of OSA is classified, and treatment options are recommended accordingly.
Treatments for Obstructive Sleep Apnea (OSA)
Treatments for OSA range from lifestyle modifications to medical interventions. The goal of treatment is to keep the airway open during sleep, ensuring a steady flow of air. The most effective treatments include:
- Continuous Positive Airway Pressure (CPAP): The gold standard for OSA treatment, CPAP involves wearing a mask connected to a machine that delivers constant air pressure, keeping the airway open.
- Oral appliances: Devices designed to adjust the position of the jaw or tongue to maintain an open airway.
- Surgical options: In severe cases, surgery may be necessary to remove excess tissue or correct anatomical abnormalities.
- Lifestyle changes: Weight loss, reducing alcohol consumption, and changing sleep positions can help reduce OSA symptoms.
- Positional therapy: For those who have trouble sleeping on their back, positional therapy can help keep them awake on their side.
Living with Obstructive Sleep Apnea (OSA)
For those living with OSA, the condition can be a daily struggle. Persistent daytime fatigue, morning headaches, and difficulty concentrating are common symptoms that can affect personal and professional life. Many people with OSA also experience mood disturbances such as irritability and depression.
Patients often rely on lifestyle adjustments, such as weight loss and improved sleep hygiene, along with medical treatments to manage the condition. For some, the introduction of continuous positive airway pressure (CPAP) therapy can be life-changing, providing immediate relief and improving sleep quality. However, it’s not uncommon for individuals to feel overwhelmed when first diagnosed with OSA, as managing the condition requires consistent adherence to therapy.
Interlinking Studies: OSA and GERD
Recent research has revealed a compelling connection between obstructive sleep apnea (OSA) and gastroesophageal reflux disease (GERD), a condition where stomach acid frequently flows back into the esophagus, causing discomfort and potential damage to the esophageal lining. Studies suggest that individuals with OSA are more likely to experience GERD symptoms, and the two conditions may exacerbate each other.
One study published in Chest (2005) found that up to 58% of OSA patients also reported GERD symptoms, compared to just 15% in the general population. The reasons for this overlap are not entirely understood, but one proposed mechanism is that the repeated airway obstructions in OSA increase intra-thoracic pressure, potentially forcing stomach contents upward into the esophagus. In turn, GERD can disrupt sleep further, creating a vicious cycle where sleep deprivation worsens both conditions.
Additionally, another study published in the American Journal of Gastroenterology (2010) highlighted that treating OSA with continuous positive airway pressure (CPAP) therapy not only improved sleep apnea symptoms but also reduced the frequency and severity of GERD symptoms. This improvement is likely due to CPAP preventing the airway obstructions that contribute to reflux events.
These findings suggest that addressing OSA in patients who also suffer from GERD could provide dual benefits, improving both respiratory function during sleep and alleviating acid reflux symptoms. It also underscores the importance of screening OSA patients for GERD and vice versa, as managing one condition could significantly ease the burden of the other.
Read Also: The Role of Web Development in Boosting Website Security
Outlook for Those with OSA
With proper diagnosis and treatment, individuals with obstructive sleep apnea (OSA) can significantly improve their quality of life. Early intervention is critical in preventing the long-term complications of OSA, such as heart disease, stroke, and diabetes. While CPAP therapy may require an adjustment period, it remains the most effective treatment for reducing apneic events and improving sleep quality.
It’s important to note that OSA is a chronic condition that typically requires ongoing management. However, with the right treatment plan and lifestyle adjustments, individuals with OSA can lead healthier, more restful lives.
In summary, obstructive sleep apnea (OSA) is a serious but treatable condition. By staying informed and seeking proper medical care, those affected can mitigate the risks and improve both their sleep and overall health.






